The Health Belief Model is a framework used in health psychology. It helps explain why people take action to prevent diseases. This model emphasizes individual perceptions and beliefs influencing health behavior. Public health professionals use it to design effective awareness campaigns. Understanding HBM helps predict how individuals respond to medical recommendations.
Developed in the 1950s, HBM remains widely used in healthcare research. It focuses on personal motivation rather than external social or economic factors. The model considers perceived risks, benefits, barriers, and health-related cues. HBM can explain behaviors like vaccination, screenings, or medication adherence. By understanding beliefs, healthcare providers improve preventive care and interventions.
The Health Belief Model consists of several core psychological components. These include perceived susceptibility, severity, benefits, barriers, and self-efficacy. It also incorporates cues to action that trigger health-promoting behaviors. This structured approach helps researchers and practitioners target behavioral changes. HBM provides valuable insights into promoting healthier lifestyles and medical adherence.
Table of Contents
Key Components of the Health Belief Model

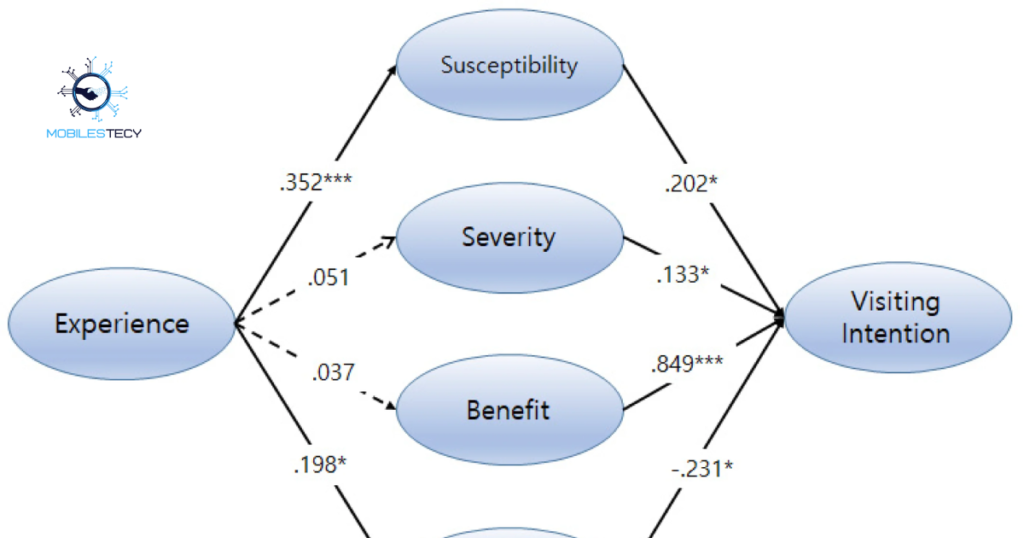
Perceived Susceptibility refers to a person’s belief about disease likelihood. Individuals who feel at risk are more likely to take preventive measures. For example, a person with family diabetes history adopts healthier lifestyle habits. Higher perceived susceptibility increases motivation to engage in protective behaviors. Addressing risk perception is essential in health education and promotion programs.
Perceived Severity involves the individual’s evaluation of health problem seriousness. It includes physical, emotional, and social consequences of illness or disease. People who recognize severe outcomes are more likely to take action. For instance, understanding lung cancer risks may reduce smoking behavior. Health campaigns emphasize severity to encourage protective health behaviors consistently.
Perceived Benefits and Barriers influence decision-making in health-related behaviors. Benefits include belief that specific actions reduce health risks effectively. Barriers include costs, inconvenience, fear, or social stigma preventing action. Reducing barriers increases likelihood of engaging in preventive behaviors successfully. Health educators focus on highlighting benefits and overcoming obstacles simultaneously.
Cues to Action and Self-Efficacy
Cues to Action trigger people to adopt health-promoting behaviors actively. They can be internal, like symptoms, or external, like media campaigns. A reminder text to schedule vaccinations is a practical example. Providing clear cues enhances adoption of preventive measures consistently.
Self-Efficacy refers to confidence in performing a specific health behavior. Even if risks are high, low confidence can prevent effective action. Programs that build self-efficacy increase adherence to treatment or lifestyle changes. Techniques include coaching, goal-setting, and providing skill-building opportunities.
Applications of the Health Belief Model

The HBM is widely used in vaccination and immunization programs effectively. It identifies populations with low perceived susceptibility or benefit perceptions. Targeted messaging can correct misconceptions and increase vaccination rates significantly. For example, COVID-19 campaigns addressed personal risk and vaccination advantages directly. Understanding HBM principles improves reach and engagement in preventive programs.
Screening and early detection programs also apply HBM frameworks effectively. HBM explains why some individuals avoid cancer screenings or medical tests. Interventions reduce barriers, reinforce benefits, and provide actionable reminders effectively. Personalized education materials and appointment reminders increase participation rates significantly. Cues to action are essential to motivate people to undergo screening regularly.
Lifestyle modification and chronic disease management programs use HBM insights. Diet, exercise, smoking cessation, and medication adherence depend on personal beliefs. Programs enhance self-efficacy and emphasize benefits while reducing perceived obstacles. Example includes hypertension management using coaching, meal planning, and exercise programs. HBM-based interventions improve long-term health outcomes and behavioral consistency effectively.
Strengths of the Health Belief Model
HBM provides a simple, clear framework for understanding health behaviors effectively. Its constructs allow practitioners to predict behavior and plan interventions efficiently. The model is easy to apply in public health research and practice.
The model may oversimplify complex health behaviors into single perception factors. Individual motivations are often influenced by overlapping cognitive, emotional, and social determinants. Ignoring these interactions can reduce intervention effectiveness.
Limitations of the Health Belief Model
One limitation is its focus on cognitive factors, ignoring social influences. Cultural norms, peer pressure, and environmental factors also shape health behavior. HBM assumes rational decision-making, which may not reflect real-life choices. Emotions, habits, and addictions often override rational health beliefs significantly.
Another limitation is its limited applicability to habitual or automatic behaviors. Routine actions like brushing teeth or taking medications are not fully explained. HBM works better for new or infrequent behaviors requiring conscious decisions. Interventions must consider additional psychological or social models for comprehensive behavior analysis.
Geographic and economic factors can also limit HBM effectiveness in populations. Individuals in rural areas or with limited resources may face access barriers. Environmental influences often interact with perceptions to determine behavior outcomes. Integrating HBM with broader frameworks addresses these additional challenges effectively.
Practical Tips Using the Health Belief Model
Design messages emphasizing personal risk and severity to motivate behavioral change. Highlight clear benefits of action while addressing common barriers effectively. Use cues to action, such as reminders or educational campaigns, consistently.
Monitor and evaluate interventions regularly to measure their effectiveness and impact. Feedback loops allow for adjustments to enhance message clarity and behavioral outcomes. Engage target populations to understand real-world barriers and perceptions fully.
- HBM explains health behaviors based on individual perceptions and beliefs clearly.
- Perceived susceptibility and severity significantly influence preventive action adoption consistently.
- Perceived benefits and barriers determine likelihood of engaging in behaviors.
- Cues to action trigger health behaviors effectively when implemented strategically.
- Self-efficacy increases adherence and confidence in performing health behaviors successfully.
Faq’s
What is the Health Belief Model in healthcare?
It is a psychological framework explaining why people adopt health behaviors.
What are the main components of HBM?
They include perceived susceptibility, severity, benefits, barriers, cues, and self-efficacy.
How is HBM applied in public health?
It guides vaccination campaigns, screening programs, lifestyle modifications, and chronic disease management.
What are HBM’s strengths in health behavior interventions?
HBM is simple, adaptable, focuses on perception, and predicts behavior effectively.
What are the limitations of the Health Belief Model?
It ignores social, environmental factors and assumes rational decision-making frequently.
Conclusion
The Health Belief Model provides a structured approach to understanding health behavior. It emphasizes individual perceptions of risk, severity, benefits, and barriers effectively. Cues to action and self-efficacy further influence decision-making and behavioral change. HBM guides interventions to improve adherence, preventive care, and lifestyle changes consistently. Understanding this model is essential for designing effective health promotion strategies successfully.
HBM is applicable across diverse health issues, populations, and cultural settings. Vaccination, screenings, chronic disease management, and lifestyle programs benefit from its principles. Tailored messages addressing beliefs and barriers result in more effective behavioral change. Healthcare providers can use it to motivate patients and improve health outcomes. Interventions built on HBM help create sustainable, long-term behavior modifications effectively.
Ultimately, the Health Belief Model remains a critical tool for public health. It bridges psychology and healthcare, predicting behaviors and informing intervention strategies. Understanding beliefs and perceptions allows practitioners to design better prevention programs. HBM-based strategies improve patient engagement, compliance, and overall population health outcomes. Its continued use highlights its relevance and adaptability in modern health promotion efforts.
Read more latest Articles on Mobilestecy.com